Although brain cancer is one of the rarest cancers, with a likelihood that it will develop during one’s lifetime being 1%, it is also one of the most challenging types to treat. It impacts more than 24,000 adults yearly and 3,400 children under the age of 15. Brain tumors are divided into benign and malignant types, with gliomas accounting for 78% of malignant cases. Among all gliomas, 30-40% are comprised of glioblastomas. These tumors are characterized by their rapid growth and are associated with a poor prognosis compared to the more indolent forms of other gliomas.
“The concept of why humans are humans is that we can communicate, function, and those get affected really early on in the disease process,” Dr. Vyshak Venur, an assistant professor of medicine at University of Washington (UW) and medical-oncologist at Seattle Cancer Care Alliance (SCCA), explains. “We are not just treating the tumor but also making sure that patients have a good quality of life and a meaningful life as much as possible.”
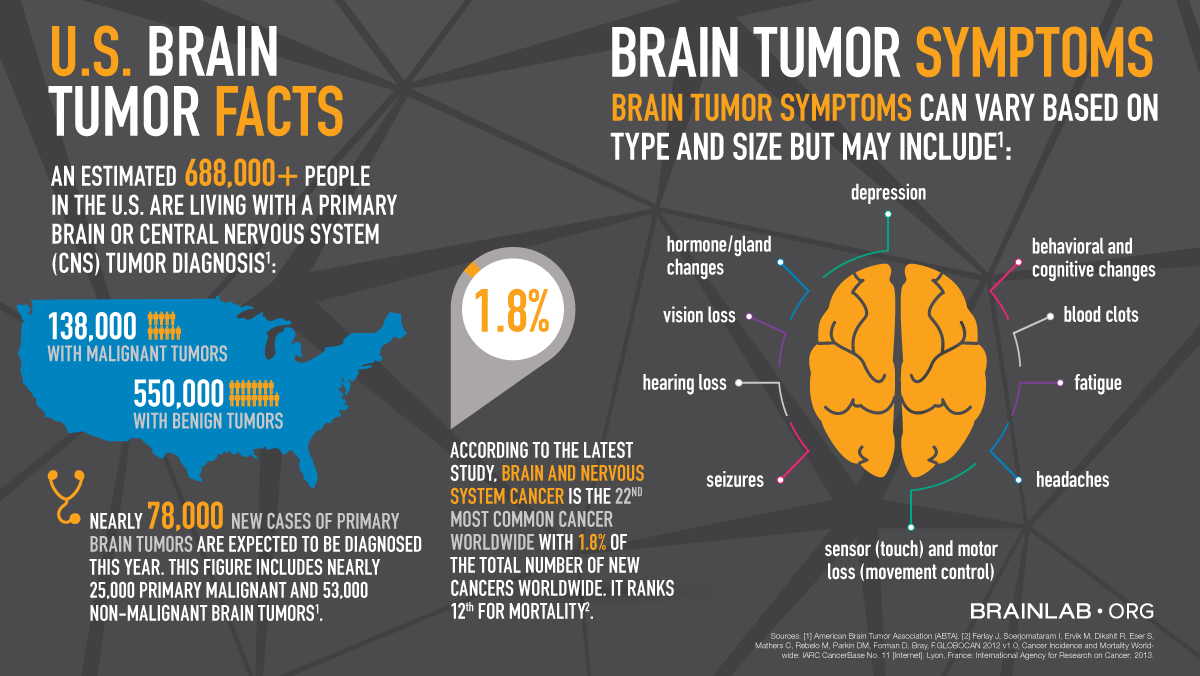
For low-grade gliomas, the most commonly presenting symptom is seizures, which brings most patients to the emergency room. A careful neurologic exam can also reveal impairments in speech, vision or muscle strength that may also prompt further tests including brain imaging studies.
Fortunately for patients, a team of highly trained providers provide them the necessary care. Typically, neurosurgeons will first perform a biopsy to confirm a diagnosis and remove as much cancer as they can to improve prognosis. Radiation oncologists can also step-in to help manage tumors, alongside medical-oncologists who administer chemotherapy and other targeted agents. Oncologists are also prescribing drugs to manage co-occurring symptoms such as brain swelling, numbness, weakness, and seizures to ensure that the treatments properly work.
“The best case scenario is when it's a benign tumor and a neurosurgeon can remove it, so the patient can live the rest of their life,“ Dr. Tresa McGranahan, an assistant professor of medicine at UW and medical-oncologist at SCCA, shares. “The most common malignant brain tumors are infiltrated, meaning that we can never cut them out, and so, some patients even in that setting can just have surveillance, for many, many years.”
For patients with low-grade tumors, they can go on to live for 10-15 years or more, so physicians care about the long-term implications of their chosen treatments. For more aggressive cases, physicians are closely monitoring short-term adverse effects such as organ and immune function. Another interesting fact about brain cancer is that it rarely metastasizes outside of the brain.
“I think brain tumors are in line with several of our other cancers where we're recognizing that actually more aggressive therapies aren't necessarily better,“ Dr.McGranahan explains. “In brain cancer, we have found that using shorter courses of radiation is just as good as using longer courses of radiation.”
Research and advancements in this field go together with an improved understanding of how the brain functions. Currently, there is a push towards testing immunotherapies and vaccines against tumors. Targeted agents are another set of agents that inhibit unfavorable biochemical pathways to prevent cell growth. Newer chemotherapies are also being tested.
May marks brain cancer awareness month and serves as a reminder that we should all be aware of sudden or unusual neurological changes such as altered vision or speech, seizures, or difficulty moving our limbs. As a rule, an impairment that occurs without explanation and is progressive should prompt us to see our caregivers for further evaluation. Learn more about ongoing initiatives against brain tumors and hear stories from current and former patients here.